IS LUMPECTOMY THE RIGHT TREATMENT FOR ME?
IS LUMPECTOMY THE RIGHT TREATMENT FOR ME?
5 Minute Read:
I have been diagnosed with breast cancer and given two choices, mastectomy and lumpectomy? Which is the right surgical choice for me?
WHAT SHOULD YOU KNOW ABOUT BREAST CANCER STATISTICS?
Breast cancer is the second most common cancer for women in the United States (following skin cancer). 1 in 8 women will be diagnosed with breast cancer in her lifetime. Due to screening mammograms and improved personalized treatment options, breast cancer survival rates have been steadily increasing in the last 10 years.
The overall five-year survival rate is 100% for stage 0 and 1, 93% for stage II, 72% for stage III, and 22% for stage IV.
WHAT ARE MY TREATMENT OPTIONS?
Surgery is the choice treatment for most early-stage breast cancer patients. Surgery is a curative treatment option done along with chemotherapy, radiation, or hormonal treatment options.
Once a woman is given a diagnosis of breast cancer, she is referred to an oncologic breast surgeon. The breast surgeon will advise her whether she is a candidate for a lumpectomy or mastectomy along with lymph node biopsy.
Lumpectomy is a partial removal of the breast containing the breast cancer whereas mastectomy is the complete removal of breast tissue. The choice between these two surgical options is individualized and based on medical recommendations along with the patient’s personal preference.
Mastectomy is still a very common surgical treatment for large size breast tumor.
Breast conservation therapy (lumpectomy) is becoming a common surgical treatment in breast cancer even in larger tumor size due to effectiveness of neoadjuvant chemotherapy (chemotherapy given prior to surgery in an attempt to reduce the tumor size).
Therefore, many patients are given two options of lumpectomy or mastectomy as part of their cancer surgical treatment.
Patients will often ask Dr. Mytien Goldberg which surgical option is the right one for them.
This blog will help guide her patients and other breast cancer patients in their decisions considering breast cancer recurrence, chronic pain, cosmetic results, surgical side effects, radiation side effects, breast reconstruction success rate, and overall patient’s satisfaction.
WHAT SHOULD A PATIENT KNOW ABOUT LUMPECTOMY?
A patient has to understand that with lumpectomy, postoperative radiation is part of the treatment. Studies have shown lumpectomy without radiation has a much higher cancer recurrence rate compare with lumpectomy with radiation (39.2% versus 14.3%).
Radiation to the remaining breast tissue will result in future breast atrophy, scarring, and changes in surrounding tissue including the skin, lung, and heart.
Studies on patient’s reported outcomes showed patient’s satisfaction depends on the volume of the lumpectomy. The larger the lumpectomy volume, the lower the satisfaction rate.
You should discuss with your breast surgeon regarding the anticipated size of the lumpectomy in relation to your overall breast size. Studies have shown lumpectomy volume of greater than 100 gm, or breast to resected tissue ratio of exceeding 10:1 will likely result in poor cosmetic results.
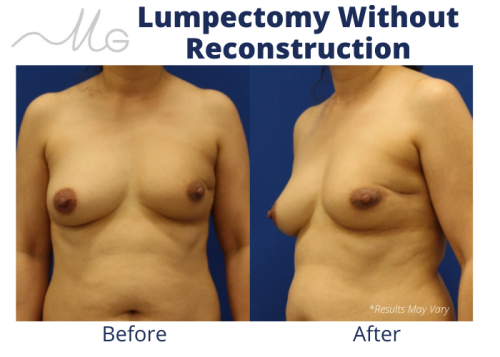
Up to 30% of patients undergoing lumpectomy reported residual deformities, such as indentation, scar retraction resulting in pain, breast asymmetry, nipple areola retraction, and loss of breast volume as illustrated in the case below.
*This patient underwent left breast lumpectomy without reconstruction and subsequent whole breast radiation. You can see the nipple retraction, scar indentation, breast asymmetry, and painful scar tissue in the lateral chest wall from radiation.
* Patient with left breast cancer underwent left breast lumpectomy and reconstruction with local tissue rearrangement, resulting in a small lift.
Tumor location also affects the cosmetic outcomes of lumpectomy. Tumor located in centrally or medial quadrant tend to have the worst aesthetic results.
The best candidate for lumpectomy will be relatively small tumor size to breast ratio, breast ptosis (sagginess), and large breast size.
In these patients, lumpectomy combined with reconstruction of the lumpectomy defect using local breast tissue will yield a pleasing aesthetic result.
This technique is becoming more and more popular as illustrated in the case below. The patient had left breast cancer with the tumor located in the upper outer quadrant.
Lumpectomy was performed 10 days prior to the definitive reconstruction using local tissue rearrangement. The reasons for performing lumpectomy prior to reconstruction is to ensure all the tumor was removed and negative margins are obtained.
It is important to get a second opinion and involve a plastic surgeon early on at the time of breast cancer diagnosis. Your lumpectomy defect can be reconstructed using your own remaining breast tissue
If you have chosen lumpectomy and do not like your results or are having residual asymmetry, pain, and scar tissue, there are several option of correcting the lumpectomy deformity. One of the most common procedure will be lumpectomy defect reconstruction using your own skin and fat from anywhere in your body.
*As illustrated in patient #1, she presents to Dr. Goldberg for with left breast pain and significant deformity. She underwent lumpectomy defect reconstruction using her own abdominal tissue called the DIEP flap.
HAVE YOU BEEN DIAGNOSED WITH BREAST CANCER? LEARN MORE ABOUT YOUR RECONSTRUCTION OPTIONS
If you are recently diagnosed with breast cancer and are looking for a plastic surgeon to perform your breast reconstruction, Dr. Goldberg is your plastic surgeon.
And if you have had breast cancer and are dissatisfied with your reconstruction results, the first step is to schedule a comprehensive in-office consultation with Dr. Goldberg. After the exam, Dr. Goldberg can create an individualized plan to address your specific concerns and answer any questions you may have.
For many women in southern California and around the country, Dr. Mytien Goldberg is the plastic surgeon of choice for breast reconstruction, revision, and correction procedures.